Hospitals and universities around the world are embracing Virtual Reality (VR) as a way for surgical trainees to practice skills and procedures in a safe, yet realistic environment. But how might the technology be used to drive the kind of peer-to-peer knowledge sharing among practicing surgeons that advances new techniques and ultimately, improves patient care?
The Johnson & Johnson Institute believes one way may be a Virtual Reality Preceptorship (VRP) Program that uses VR remote collaboration to bring the preceptor and learner surgeon together in a simulated OR environment. In this scenario, the learner is performing the procedure – instead of just observing – and the preceptor is there to share insights and cultivate dialogue. Unlike training that involves a real patient, VRP can be easily personalized to the learner’s needs. Want to go back and repeat certain procedural steps? Or stop to ask questions? You can do that. Because VRP is easily tailored to meet the learner’s goals.
Realistic Experience Fosters Dialogue, Knowledge Exchange
Gadini Delisca, MD, an orthopaedic surgeon in Rochelle, IL, took part in a VRP focused on the ANTERIOR ADVANTAGE™ MATTA METHOD™ Hip Replacement from DePuy Synthes1. Dr. Delisca was already performing the procedure but wanted to focus on incorporating the Hana® Orthopedic Table2 in the minimally invasive surgery. Alex Tauchen, MD, a hip and knee replacement surgeon in Lincolnshire, IL, was the Preceptor for the case.
According to Dr. Delisca, one of the potential advantages of VRP Program is the ability to focus in a low-pressure environment. “In a live setting, you have a patient under anesthesia and more pressure to get through it, so you don’t necessarily have time to focus on the aspects you want to master. The Virtual Reality Preceptorship Program allows you to do that.”
And this is training that can be done anytime, anywhere. The days of bulky VR sets requiring countless cords and adapters are gone. The J&J Institute offers an all-in-one VR headset that fits in a small bag, making it easily portable.
“I was surprised how realistic it was. I mean I almost forgot I was in my basement,” said Dr. Tauchen. “As the educator, I felt very connected to the learner in the environment. I would encourage everyone to try it. I think it’s unique technology with the potential to make us better.”
Today, the rapid pace of medical innovation is leading to many new procedures and techniques to improve care for patients. That’s good news, but it also puts pressure on surgeons to learn faster. The J&J Institute believes VR offers a way to help address that challenge.
“VR has the power to deliver new, exciting methods of remote collaboration and learning, “said Lauren Cruz, Senior Manager Worldwide Professional Education Technology Innovation. “We believe VRP holds the potential to help surgeons build skills and confidence with new techniques and technology that can translate to the OR– where they can benefit the patient and increase the efficiency of care.”
The J&J Institute VRP program currently offers VR 2.0 modules in Orthopaedics (Joint reconstruction, trauma, extremities) and Electrophysiology. More modules are slated to become available in the coming months.
1. The Anterior Approach, as described by Dr. Joel Matta, utilizes a tissue sparing philosophy. DePuy Synthes has collaborated with Joel Matta, M.D., to build a comprehensive training and education program around the Anterior Approach.
2. The Hana® table allows precise control of patient positioning, manipulation and traction during this minimally invasive hip replacement surgery and provides better access to the hip joint for improved alignment and positioning of the implant.
Quelle:
https://jnjinstitute.com/en-us/news/virtual-reality-preceptorship-program-personalizes-learning









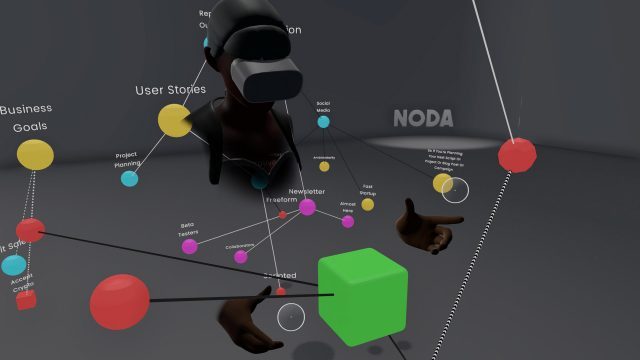
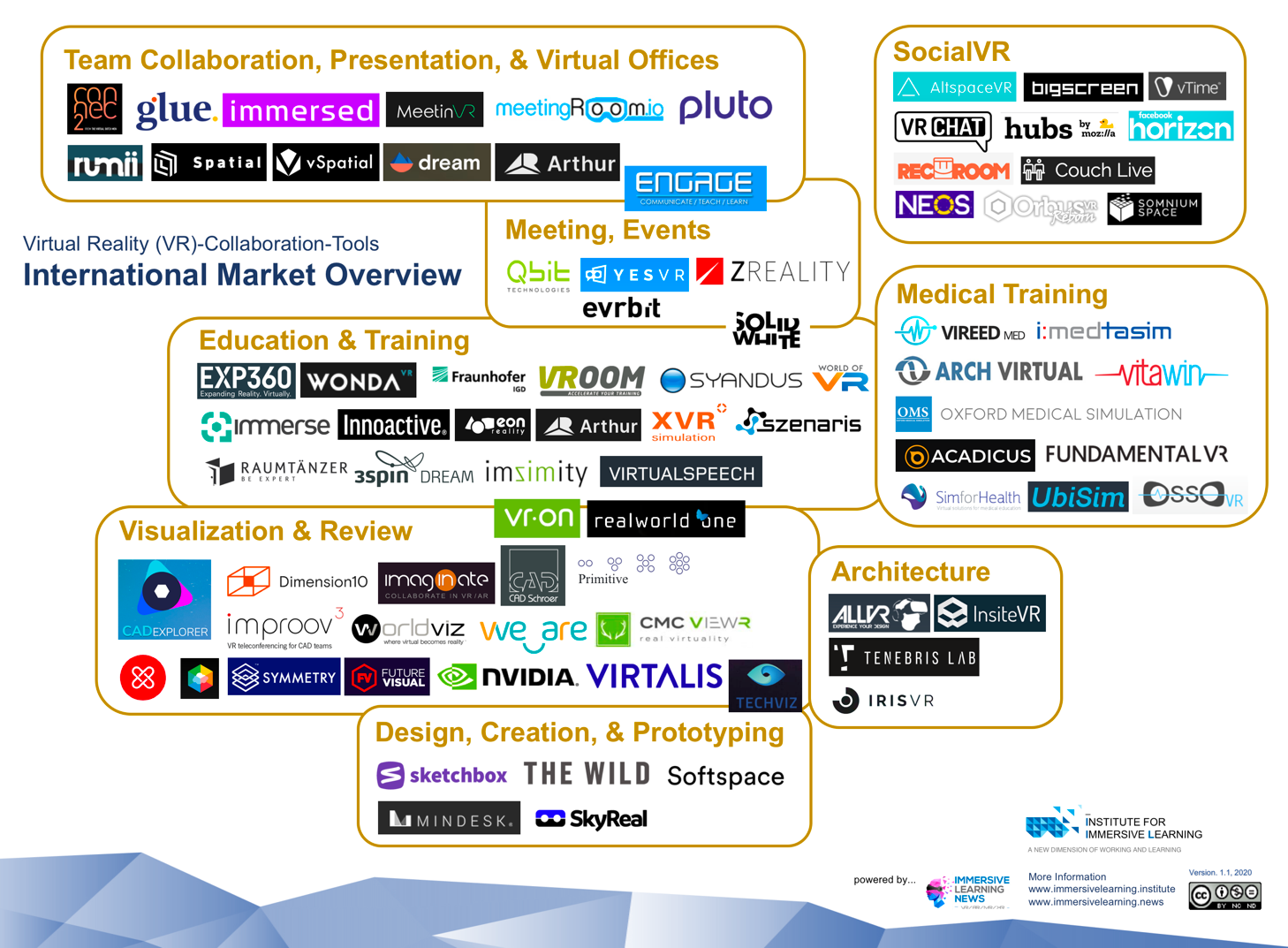
 VR Collaboration ist in aller Munde, immer mehr Beispiele, Standard-Software-Lösungen kommen auf den Markt. Die großen Hersteller legen alle nach, um Arbeiten und Lernen von überall und das in einer virtuellen Welt zu ermöglichen. Ob Beratungs-, Kreativ- oder Trainingsprozesse dies spielt keine Rolle mehr, nur wie gestaltet man diese effizient und wie müssen diese begleitet werden.
VR Collaboration ist in aller Munde, immer mehr Beispiele, Standard-Software-Lösungen kommen auf den Markt. Die großen Hersteller legen alle nach, um Arbeiten und Lernen von überall und das in einer virtuellen Welt zu ermöglichen. Ob Beratungs-, Kreativ- oder Trainingsprozesse dies spielt keine Rolle mehr, nur wie gestaltet man diese effizient und wie müssen diese begleitet werden.